Oral and Maxillofacial Pathology


What is Oral and Maxillofacial Pathology?
Oral and maxillofacial pathology deals with the diagnosis and management of diseases affecting the oral and maxillofacial regions.
The pathology seen in the oral region that Dr Schenberg manages include:
- Red, white and pigmented lesions of the oral mucous membrane.
- Dysplastic and malignant diseases of the oral mucosa and lips.
- Lesions within the soft tissues of the mouth and adjacent structures.
- Lesions within the jaw bones including cysts and benign and malignant tumours.
- Jawbone lumps and exposed jaw bone lesions.
- Salivary gland lesions (not including the parotid glands).
- Infectious diseases, dental abscesses, impacted wisdom teeth.
For patients, it is important not to jump to the conclusion that any lesion of the mouth is a cancer. Cancers of the oral cavity make up only a very small percentage of all oral and maxillofacial pathology lesions.
Diagnosis
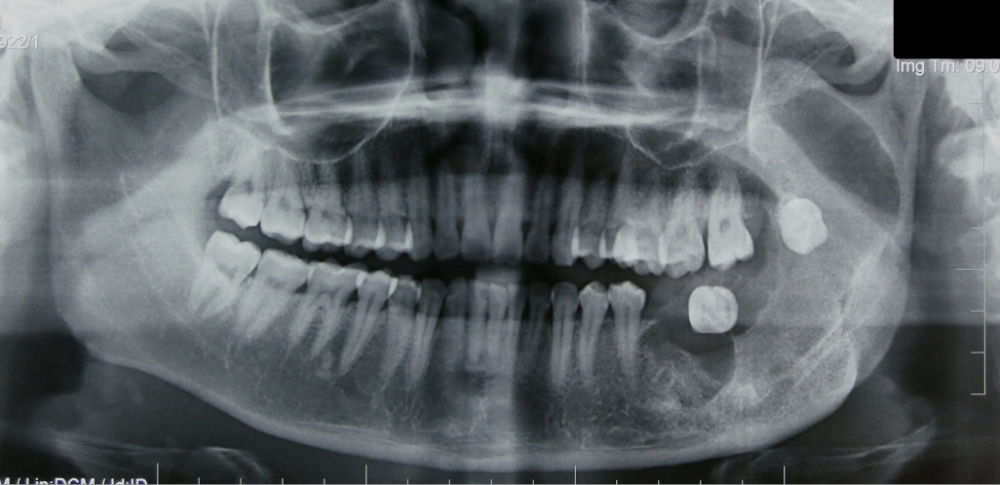
Diagnosis involves first hearing the patient’s history of the condition. Then examining the patient and observe the location, visual characteristics and feel of the lesion. Next investigations may be arranged. These investigations could include:
- Special imaging such as an OPG xray, a cone beam CT scan or a standard CT scan.
- An incisional biopsy where a small sample of the lesion is removed and sent for microscopic examination and diagnosis with a pathology service.
- An excisional biopsy may be performed if the lesion is small, and all the lesion is removed and sent for microscopic examination and diagnosis with a pathology service.
- Before a biopsy is performed the area is anaesthetised with a local anaesthetic.
Treatment
Once a diagnosis has been made only then can the appropriate treatment be arranged. The type of surgery, if needed, will depend on the diagnosis. The treatment may range from observation to surgery.
Each type of lesion has its own characteristics and hence the appropriate treatment that gives the best results will depend on that diagnosis. Treatment is discussed at the appointment after the diagnosis has been determined.